In the past several months, workers at Moss Park’s safe consumption site have been forced to call paramedics for drug users in cardiac distress more times than ever before.
On Wednesday, three site staff told TorontoToday the suspected cause: a dramatic increase in veterinary tranquilizers in the downtown fentanyl supply.
“We have never called EMS more frequently for anything,” said Sarah Greig, director of substance use and mental health for the Moss Park Consumption and Treatment Service (CTS).
“We’re worried that people are going to bottom out or have their heart stop.”
While one veterinary tranquilizer, xylazine, has been present in a portion of the downtown fentanyl supply for several years, experts said a second, called medetomidine, began showing up in January.
Combined, experts said the rate of veterinary tranquilizers in Toronto's fentanyl supply has never been higher.
In its latest drug report, Toronto’s Drug Checking Service found 81 per cent of expected fentanyl samples it tested contained xylazine or medetomidine — tranquilizers typically used to sedate dogs, horses or cattle for surgeries and other procedures.
When a sample is submitted to the drug checking service, the sender shares the type of drug they believe was purchased. The free-to-use service then tests the substance to identify the drug and the presence of other potential contaminants.
Workers said veterinary tranquilizers in fentanyl — sometimes referred to as “tranq” or “tranq dope” — pose a big challenge in their efforts to help keep people alive.
At least 99 xylazine deaths since 2021
Between January 2021 and June 2024, at least 99 people died in Ontario as a result of drug toxicity directly attributable to xylazine, according to information provided by the province’s Office of the Coroner.
During the same 3.5-year period, an additional 275 people in Ontario died of drug toxicity where xylazine was detected post-mortem and may have played a role.
A spokesperson for the Office of The Coroner said the death counts are believed to be underestimates, as data lags due to the time required to identify the cause of death in each case.
In recent months, Moss Park CTS staff told TorontoToday they’ve seen a significant increase in incidents where drug users’ heart rates have become dangerously low, irregular or have stopped entirely.
Staff suspect the tranquilizers — which are not approved for use in humans — are to blame.
Whereas opioid overdoses can often be reversed using naloxone, this remedy is not effective for veterinary tranquilizers, said Hayley Thompson, managing director of Toronto’s Drug Checking Service.
A spokesperson for Toronto Public Health added that when the drug supply is unpredictable and toxic, people who use drugs are at greater risk for an overdose because the drugs may be different or more potent than expected.
Why are there tranquilizers in fentanyl?
Thompson said she doesn’t know for certain why veterinary tranquilizers are being added to fentanyl in Toronto.
She said she suspects some drug creators are incorporating the substances to try to make the effects of fentanyl last longer.
The drug, which is about 20 to 40 times more powerful than heroin, offers a quick high then a state of calm for one or two hours, according to the federal government.
Evan Moore, a community health worker at Moss Park CTS said it’s possible the tranquilizers are showing up more frequently because of disruption in the fentanyl market. Such disruptions can occur because of a drug bust or the death of a supplier, he said.
Within the context of an unregulated supply of drugs, Moore said disruptions make it more challenging for drug users to obtain substances from sources they trust.
It is not clear how drug makers are obtaining the veterinary tranquilizers.
Lori Ahronson, senior manager of marketing for the Canadian Veterinary Medical Association told TorontoToday in an emailed statement that xylazine and medetomidine can only be dispensed with a prescription from a veterinarian.
TorontoToday asked the Toronto Police Service where fentanyl containing veterinary tranquilizers is coming from but did not receive a response prior to publication.
Tranqs and ‘social disorder’
Moss Park CTS staff said the lack of a regulated drug supply is making life more challenging for drug users and for the community at large.
Over the past few weeks, Moore said they’ve seen many clients acting out of character — delirious, unusually rageful or like they’re in a “fugue state.”
He said staff suspect it's the result of veterinary tranquilizers or benzodiazepines in the fentanyl supply. “Benzos” are another type of tranquilizer which has depressant effects on the central nervous system.
When individuals ingest such drugs, it can leave them acting like someone experiencing a mental health crisis, Greig said.
A drug user told her yesterday that when she does “tranq dope” she dreams she’s talking to someone. When she comes to, she realizes nobody is there.
Greig said staff have witnessed drug users appear like they are “sleep walking” or interacting with things “the rest of us could not perceive."
Taking contaminated fentanyl of this kind can contribute to drug users becoming lost or missing health appointments, she said.
Contaminated drugs can also make it more challenging for paramedics, social workers and friends and family of drug users to know how to intervene.
“People are being restrained more frequently when they’re presenting with this bizarre behaviour,” Greig said, adding this experience can be traumatizing for some drug users.

Concern about safe consumption site closures
Thompson said it’s particularly alarming this escalation in drug contamination is happening now.
At the end of March, five of Toronto’s safe consumption sites will be shuttered as a result of new provincial rules.
While the provincial government said the new safe consumption site laws will increase safety by decreasing drug use near schools and daycares, Greig said she’s worried the changes will increase the number of fatal overdoses.
In December, she said she helped save the life of a man who took drugs at the safe consumption site. She said the man may have otherwise died if he had used drugs alone.
Grieg said the man’s heart stopped beating so she performed chest compressions for at least six minutes.
“I’m so grateful that we were here in real time because he’s alive and he’s made many life changes since then,” she said.
Grieg said without supervised consumption, drug users “often don't live long enough to make it to the hospital.”
Between 2020 and 2023, more than 500 people died each year in Toronto from opioid-toxicity related deaths, according to Public Health Ontario.
This January alone, paramedics were called for 250 suspected opioid overdoses, of which 12 were fatal.
Encouragement to test drugs
Thompson said drug users can reduce the risk of taking contaminated substances by getting their drugs tested.
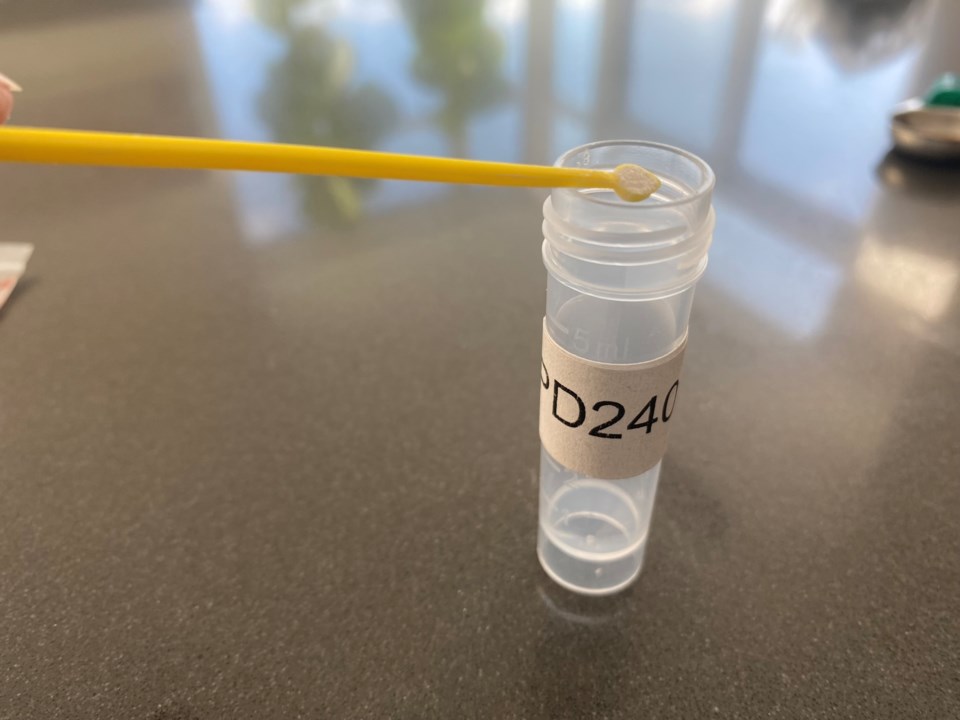
To use Toronto’s Drug Checking Service, a person can bring a small amount of drugs — far less than the size of a pill — or drug equipment, such as a used needle with a small amount of liquid, to one of ten drop-off locations.
The service picks up the samples, tests it and within one business day provides information about what’s in the drug, according to Thompson.
The service is anonymous and information can be provided to drug users by text, email, the site’s online portal or in-person at the drop-off location.
After the closure of the five safe consumption sites, drug checking services will remain available at Street Health (338 Dundas St. E.) and Parkdale Queen West Community Health Centre (1229 Queen St. W.), according to Toronto Public Health.
As for how the broader public can help neighbours who may be experiencing adverse effects of drugs, Greig said to telephone 211 in the event of a mental health crisis and 911 if it’s a medical or safety emergency.
